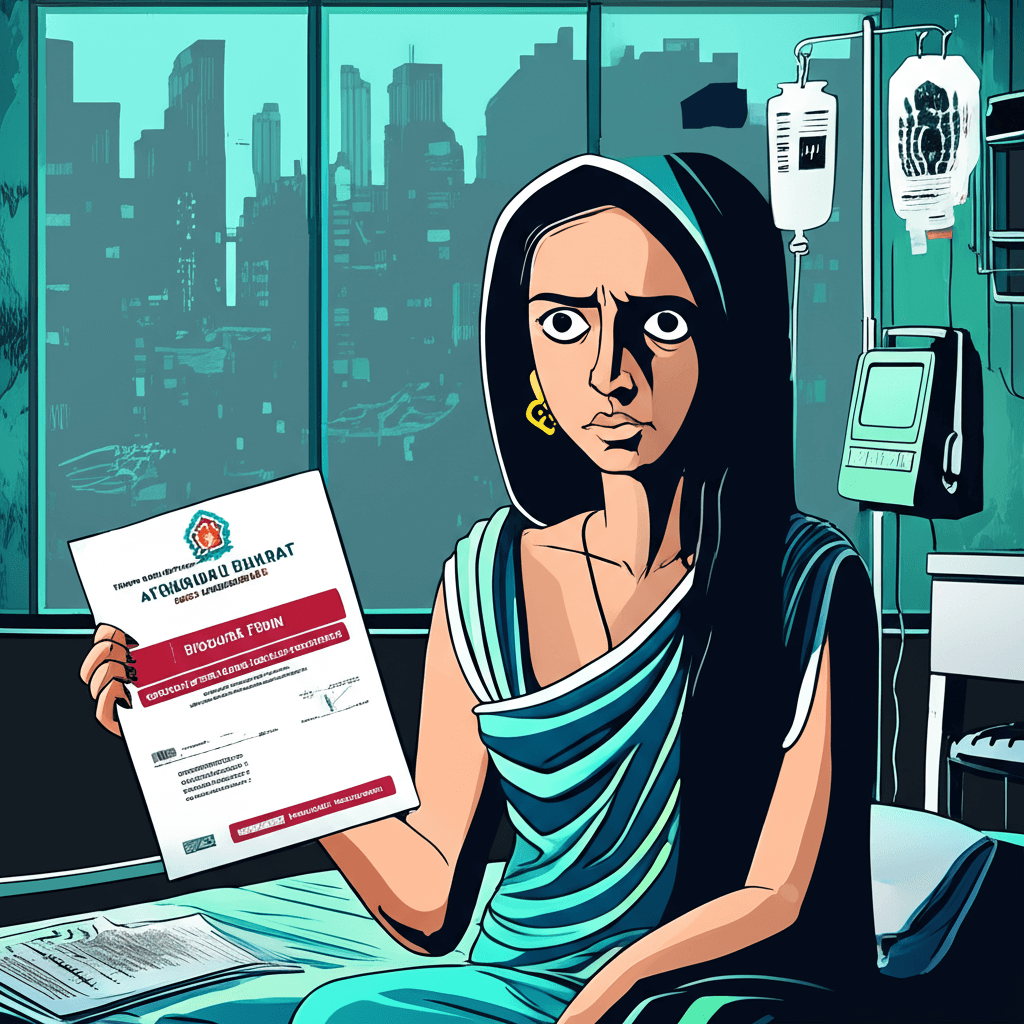
A Mumbai Woman’s Ordeal Highlights Deep Flaws in Ayushman Bharat’s Healthcare Promise
A recent incident from Mumbai has thrust the Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (PM-JAY) under harsh scrutiny, revealing troubling realities beneath India’s flagship health insurance scheme. A woman from Mumbai, attempting to use the scheme’s promise of free cashless treatment worth ₹5 lakh for her ailing father, found herself navigating a nightmarish tangle of denial, misinformation, and poor hospital affiliation. Her experience has reignited critical questions about the scheme’s accessibility, transparency, and actual impact on India’s vulnerable citizens.
What Happened: The Mumbai Experience
Early one morning, the 67-year-old retired banker’s sudden medical emergency prompted his daughter to call 24 hospitals listed under Ayushman Bharat across Mumbai, Thane, and Navi Mumbai. Instead of swift, lifesaving help, she encountered:
– Ten hospitals denying any affiliation with the scheme. – Six hospitals completely unreachable — with phone lines either ringing endlessly or out of service. – Others imposing baffling conditions — like confining coverage validity only to ICU care or specific treatments such as oncology.
Distressed and frustrated, she posted a video on X (formerly Twitter) questioning the system’s integrity: “If a family like ours—educated, internet-savvy—cannot access the scheme in a crisis, then how are poor families and daily wage workers supposed to navigate this complexity?”[source](https://www.freepressjournal.in/mumbai/not-a-single-hospital-took-us-in-mumbai-woman-calls-5-lakh-ayushman-bharat-claim-a-joke).
Her father’s health crisis was ultimately unmanaged under the scheme, leaving the couple’s hopes and the government’s flagship campaign hanging in the balance.
The Promise Vs. Reality of Ayushman Bharat
Launched in 2018 to provide cashless health insurance coverage of up to ₹5 lakh per family annually, Ayushman Bharat aims to cover over 50 crore of India’s most vulnerable citizens. The scheme promised to reduce the financial burden of healthcare and enhance access to quality treatment. However, ground realities suggest a stark contrast:
– Many hospitals empaneled officially may not honor or even recognize the scheme reliably. – The absence of an efficient grievance redressal mechanism leaves patients stranded during emergencies. – Well-documented cases of fraud and administrative lapses undermine the objective of universal coverage.[source](https://www.deccanherald.com/india/356-lakh-claims-worth-rs-643-cr-rejected-for-frauds-under-ayushman-bharat-scheme-3442492).
Fraud and Mismanagement: A Two-Edged Problem
Ayushman Bharat’s challenges are multi-layered. While some hospitals refuse to admit patients under the scheme, others have been caught inflating or faking claims:
– Over 3.56 lakh claims worth ₹643 crore were rejected for fraud; 1,114 hospitals were removed from empanelment due to fraudulent practices. – Penalties exceeding ₹122 crore were levied on errant hospitals. – States like Punjab, Haryana, and Himachal Pradesh reported massive fake claims, worsening the trust deficit. Despite the government’s fight against misuse through an anti-fraud unit and policy measures, such systemic issues put immense strain on genuine beneficiaries.[source](https://timesofindia.indiatimes.com/city/chandigarh/fake-claims-in-ayushman-bharat-rs-562-4cr-fraud-health-insurance-claims-in-india-74cr-of-them-from-punjab-haryana-himachal-pradesh/articleshow/118181621.cms).
Expert Insights: Why the Scheme Falters on the Ground
Healthcare experts and policy analysts point to several core reasons for Ayushman Bharat’s gap between promise and delivery:
1. Poor Hospital Network Management: Lack of routine verification and frequent disconnect between official empanelment lists and on-ground hospital practices. 2. Information Asymmetry: Patients often receive contradictory information about scheme eligibility and treatment scope. 3. Complex Claim Processes: Red tape and demanding documentation discourage timely usage. 4. Infrastructure and Human Resource Limitations: Deficient capacity to handle emergencies in empaneled hospitals. 5. Digital Divide: Navigating the scheme via apps or helplines remains inaccessible to many vulnerable populations.
Some experts advocate for stronger monitoring, transparent dashboards for beneficiaries, and simplified protocols that empower patients rather than confuse them.
What Can Be Done: Practical Solutions and Citizen Advice
To reclaim the trust and potential of Ayushman Bharat, the following steps are critical:
– Robust Hospital Audits: Regular checks to ensure hospitals honor their empanelment commitments and clear removal of non-compliant facilities. – Accessible Helpline and Support: 24/7 real-person assistance should be mandated to help beneficiaries during emergencies. – Transparent Online Portals: Real-time verification of empanelled hospitals with user reviews can aid patients in decision making. – Public Awareness Campaigns: Demystifying the scheme for grassroots users, explaining eligibility, claim process, and hospital contacts. – Simplified Procedures: Hospitals and patients should encounter minimal paperwork to speed up admission and cashless treatment.
For citizens, the best tips include:
– Confirm hospital empanelment independently via official Ayushman Bharat portals. – Keep scheme helpline numbers handy when seeking treatment. – Record all communications with hospital officials for grievance redress. – Use social media responsibly to raise awareness of genuine issues but also verify information.
The Road Ahead: A Call for Accountability
The Mumbai woman’s poignant question echoes nationwide: If educated families with internet access can find Ayushman Bharat “a joke,” how will the vast majority—rural families, the elderly, the illiterate—access it when needed most?
Ayushman Bharat remains India’s most ambitious healthcare scheme. Its success or failure will have profound implications for universal health coverage and social equity. Ministries at the central and state level, healthcare providers, and civil society must unite in urgent reforms that prioritize patient welfare and transparency over bureaucratic accomplishment.
Without these, experiences like the one from Mumbai risk repeating painfully—turning the promise of ₹5 lakh coverage into an empty slogan. Only accountable, citizen-centric action can transform Ayushman Bharat into the lifeline it was envisioned to be.
For more insights on healthcare policies and citizen rights under Ayushman Bharat, explore government resources and trusted healthcare watchdog reports regularly.